Melanoma Removal Surgery
Melanoma is a type of skin cancer. It starts in the cells called melanocytes that give skin a tan or brown color. Because of this, it often starts as a mole or dark spot on the skin. It spreads faster than many other types of cancer. It's important to get this treated because it can be life threatening.
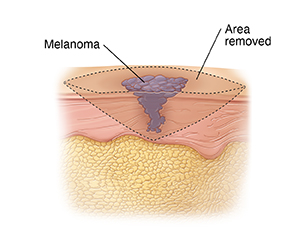
Melanoma is diagnosed with a biopsy. This is when a tiny piece of the abnormal skin is removed and tested for cancer cells. Once a diagnosis is made, a larger area around the melanoma is also removed. This is called a wide local excision. If the cancer is found early, when it's small and hasn't spread, it has a high chance of being cured.
You may need a skin graft or flap to cover and replace the skin that is removed in surgery.
Removing lymph nodes
Lymph nodes are small clumps of tissue that are part of the body’s immune system. If melanoma spreads, it often goes to nearby lymph nodes first.
The sentinel nodes are the first lymph nodes tumor cells spread into. These are the first place that cancer is likely to spread. Depending on the thickness of your tumor, the sentinel nodes may need to be removed and checked for cancer cells. A sentinel node biopsy is a test that's often done during surgery to remove melanoma. This test helps the surgeon know which lymph nodes to remove. If you're going to have a sentinel node biopsy, your surgeon can tell you more about what to expect. Locating the sentinel lymph node (sentinel lymph node mapping) is best done before the wide local excision.
If you have lymph nodes that look swollen (enlarged) on an imaging test such as a CT scan, or can be felt during an exam, a needle biopsy might be done to see if they contain melanoma cells. If they do, all of the lymph nodes in the area might be removed. This is called a lymph node dissection.
Risks and complications
Risks and possible problems from melanoma surgery include:
-
Bleeding
-
Infection
-
Scarring at the surgery site
-
Problems with the skin graft
-
Not removing all of the cancer, which may mean more treatment is needed
-
Risks of anesthesia
-
Fluid build-up and swelling in an arm or leg (lymphedema) if many lymph nodes were removed
Preparing for surgery
Get ready for the surgery as you’ve been told by your healthcare team. Be sure to:
-
Tell your healthcare provider about all medicines you take. This includes over-the-counter and prescription medicines, street drugs, marijuana, vitamins, herbs, CBD, and other supplements. It also includes any blood thinners or daily aspirin. You may need to stop taking some or all of them before surgery.
-
If you're getting general anesthesia, follow any directions you are given for not eating or drinking before surgery.
-
If you’re having a sentinel node biopsy, you may be given an injection of harmless blue dye or a small amount of radioactive substance to locate the sentinel lymph nodes the day before surgery.
The day of surgery
The surgery may take many hours, depending on what's done. You will likely go home the same day.
Before surgery
-
An IV (intravenous) line is put into a vein in your arm or hand. It's used to give you fluids and medicines.
-
You'll be given medicine to keep you from feeling pain during surgery. This may be general anesthesia, which puts you into a deep sleep. A tube may be put into your throat to help you breathe. Or, you may be sedated, which makes you relaxed and sleepy. If you have sedation, local anesthesia will be used to numb the area being worked on. If the surgery is done to remove a smaller skin tumor, you might only need local anesthesia. The surgeon and anesthesiologist will discuss your choices with you.
During surgery
-
If a sentinel node biopsy will be done, a harmless blue dye or a small amount of radioactive substance is injected into or near the tumor. This helps the healthcare provider find the lymph nodes where cancer may have spread.
-
A cut (incision) is made at the tumor. The tumor is removed along with some of the normal tissue around it. This helps make sure that any cancer cells that may have spread to nearby skin are removed.
-
One or more lymph nodes near the tumor may be removed. These are checked for cancer cells (a sign that cancer has spread).
-
The incision may be closed with stitches or staples. In some cases, a skin graft or flap may be needed to help close the site. This can come from your own body, a donor, or manmade sources. The healthcare provider will discuss the different types of grafts with you before the surgery.
After surgery
If you had only local anesthesia, you can go home shortly after surgery. If you had general anesthesia, you’ll be taken to a recovery room to wake up. You may feel sleepy and nauseated. If a breathing tube was used, your throat may be sore at first. You’ll be given medicine to manage pain. When it’s time for you to go home, you'll need an adult family member or friend ready to drive you.
Recovering at home
Once at home, follow the instructions you’ve been given. Your healthcare provider will tell you when you can return to your normal routine. Be sure to:
-
Take all your medicines as directed. Be sure you know how to use your pain medicine and what side effects you should watch for.
-
Care for your incision as instructed.
-
Don’t do heavy lifting or strenuous activities as directed.
-
Don’t drive until your healthcare provider says it’s OK. Don’t drive if you’re taking medicine that makes you sleepy or drowsy.
-
Follow your healthcare provider’s guidelines for showering. Don’t swim, take a bath, use a hot tub, or do other activities that cover the incision with water until your provider says it’s OK.
When to call your healthcare provider
Call your healthcare provider right away if you have any of the following:
-
Chest pain or trouble breathing (call 911)
-
Fever of 100.4° F ( 38°C ) or higher, or as directed by your healthcare provider
-
Chills
-
Symptoms of infection at an incision site, such as increased redness or swelling, warmth, worse pain, or drainage
-
Problems with the skin graft or flap
-
Pain that can't be controlled with medicine
-
Warmth, redness, or swelling in an arm or leg
Be sure you know how to reach your healthcare provider any time you need help, including after office hours and on weekends and holidays.
Follow-up
You will have follow-up visits so your healthcare provider can see how well you’re healing. If needed, stitches or staples will be removed at one of these visits. You and your provider can also discuss next steps and other treatments you may need.