Intraperitoneal (IP) Therapy for Cancer
Intraperitoneal (IP) therapy is used to treat cancer in the abdomen and pelvis. This includes cancer of the ovary, and less often, gastrointestinal cancer. With this therapy, chemotherapy (chemo) is put directly into the belly (abdominal cavity). Chemo is medicine used to kill cancer cells. IP therapy is often done with other treatments. These may include surgery or chemo given through a vein.
How IP therapy works
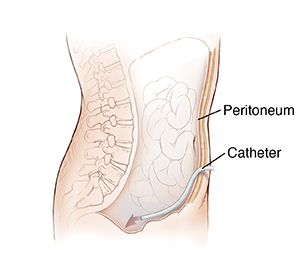
Medicine is given through a peritoneal port. It is connected to a small plastic tube (catheter) that is placed into the space between the muscles and organs in the belly. This is called the peritoneal space. The chemo stays inside this space for hours or days, depending on the treatment plan. It comes into contact with the tissues. This lets the chemo directly kill the cancer cells and help shrink tumors there.
Getting ready for IP therapy
Before you get IP therapy, you will need to have a special port put in. This port is called a peritoneal port. It is a small chamber that is placed under the skin surgically. A thin, flexible tube called a catheter is placed into the abdominal cavity and attached to the port. The port and catheter are underneath your skin. The port is accessed by a special needle. IP therapy is injected through this port. The procedure to put in a port takes about 1 to 2 hours. It is done 2 to 14 days before IP treatment is given.
IP therapy can also be given through a surgically placed IP catheter. For this, 1 end of the catheter is attached to a wider piece of tube that stays outside the body.
Having IP therapy
You lie down on a bed or table. A small tube called an IV (intravenous) line is put into a vein in your arm or hand. This line gives you fluids and medicines. A topical anesthetic is put on your port site to numb the area. A special needle with a tube attached is put into your port. Then medicine is given through the tube. It goes into the port and through the attached catheter into your belly (abdomen) area. You may feel some cramping while the medicine is being given. You will be asked to move from side to side to make sure the fluid spreads throughout your belly. This therapy can take about 2 to 4 hours. The medicine stays in your body for a few days. Then it is slowly absorbed by the body. The port needle is removed before you go home.
After IP therapy
IP therapy adds fluid to your belly. So you may feel some pressure and bloating. It may help if you walk around after treatment, or sit upright. Wear comfortable loose-fitting clothing with a stretchy waistband for the next few days. As the fluid is absorbed by your body, you may need to pee more often. You may also be told to drink a lot of fluids during this process.
Possible side effects of IP therapy
Chemo medicines are used during this treatment. So the side effects of this treatment are similar to those of chemo. Side effects will depend on the type of chemo given, but they can include:
-
Tiredness (fatigue)
-
Increased risk of infections
-
Belly pain
-
Mouth sores
-
Itchy, dry skin
-
Changes in skin color
-
Hair loss
-
Changes in or loss of nails
-
Nausea and vomiting
-
Loss of appetite
-
Loss of sexual desire
-
Bleeding problems
-
Easy bruising or bleeding
-
Numbness, tingling, and pain in the hands and feet
Your healthcare provider can tell you more about the side effects you might expect. They can tell you when to report them and how to manage them.
When to call your healthcare provider
Call your healthcare provider right away or get immediate medical care if you have any of the following:
-
Fever of 100.4ºF ( 38ºC) or higher, or as advised by your provider
-
Redness, swelling, or pain that gets worse around the port site
-
Unexplained bleeding
-
Extreme tiredness that doesn’t get better between treatments
-
Dizziness, lightheadedness
-
Constant feeling of being cold
-
A cut or rash that swells, turns red, feels hot or painful, or starts to ooze
-
Any other signs or symptoms as advised by your provider
Call 911
Call 911 right away if you have any of these:
-
Shortness of breath, wheezing, or trouble breathing
-
Fast, irregular heartbeat
-
Chest pain
Checking your progress
During your treatment, you’ll have routine follow-up visits and more testing done with your healthcare provider. These let your provider keep track of your health and response to the treatment. After treatment ends, you and your provider will talk about your treatment results. You’ll also talk about whether you need more cancer treatments.
Risks and possible complications
These include:
Your healthcare provider will tell you about other risks that may apply to you.