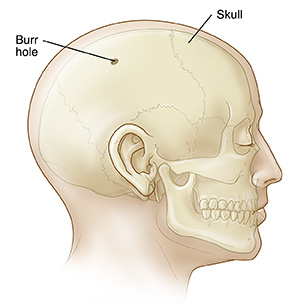
Having a Burr Hole Procedure
Burr holes are dime-sized holes that a neurosurgeon makes in the skull. Burr holes are used to help relieve pressure on the brain when fluid, such as blood, builds up and starts to press on brain tissue. This blood buildup is dangerous. As the blood builds, it pushes against the brain. If the blood starts to squeeze (compress) the brain, it can lead to symptoms such as paralysis, confusion, coma, or even death if not treated.
What to tell your healthcare provider
Tell your healthcare provider about all the medicines you take. This includes blood thinners and over-the-counter medicines such as aspirin. Tell your healthcare provider about any recent changes in your health, such as a fever.
Tests before your procedure
You may need some tests before the procedure, such as a CT scan or MRI. This is done to get more information about the location and amount of fluid around your brain.
Getting ready for your procedure
In some cases, a burr hold procedure happens as an emergency treatment. If the procedure is planned, talk with the healthcare provider about what you should do to get ready. You may need to stop taking some medicines ahead of time, such as blood thinners. If you smoke, you’ll need to stop before your surgery. Smoking can delay healing. Talk with your healthcare provider if you need help to stop smoking.
Also, make sure to:
-
Ask a family member or friend to take you home from the hospital. You can’t drive yourself.
-
Follow any directions you are given for not eating or drinking before your surgery.
-
Follow all other instructions from your healthcare provider.
You will be asked to sign a consent form that gives your permission to do the procedure. Read the form carefully. Ask questions if something is not clear.
On the day of your procedure
The exact details of your procedure may vary. Ask your neurosurgeon what your procedure will be like. In general, you can expect the following:
-
Just before the procedure, you’ll have an IV (intravenous) line put in your arm or hand. You will get a medicine through the IV to make you relaxed and sleepy. Or you will get a medicine to make you sleep fully (general anesthesia).
-
During the procedure, a healthcare provider will carefully watch your vital signs, such as heart rate and blood pressure.
-
Hair will be trimmed in the area of your scalp.
-
The surgeon will inject numbing medicine into your scalp.
-
The surgeon will make a cut (incision) in your scalp.
-
Using a special drill, a surgeon drills one or two small holes in the skull. This lets the surgeon reach the dura. This is the outermost layer of membrane around the brain.
-
The surgeon then opens the dura and drains any excess fluid to reduce pressure inside the skull. The space where the blood was collected will be washed with saline.
-
The surgeon may then place a short-term (temporary) drain to keep draining the fluid. A metal plate may be placed over each hole and held in place with small screws. The skin is closed with staples or stitches. Skin glue is sometimes applied.
After your procedure
After your procedure, your healthcare provider will carefully watch your vital signs. You may need to stay in the hospital for a few days as you recover. Your original symptoms may go away quickly from the reduced pressure on your brain.
You may have some pain at the site of your scalp incision. Over-the-counter pain medicines are often enough to treat it.
You should be able to drink and eat normally after the surgery. You can go back to most of your activities as soon you are able. Don’t do any activities that might cause a blow to the head. Don’t drive again until your healthcare provider says it's OK. Your healthcare provider may give you more instructions about caring for your wound or about your medicines. Go to all your follow-up appointments. You may need to have a drain or stitches removed. You may need one or more head CT scans. These are done to be sure that the blood or fluid over the brain did not come back.
When to call your healthcare provider
Call your healthcare provider right away if you have any of these:
-
A fever of 100.4⁰F (38⁰C) or higher, or as advised by your provider
-
Seizure
-
Muscle weakness
-
Confusion
-
Stiff neck
-
Swelling, redness, or opening of your scalp incision