Surgery for an Undescended Testicle
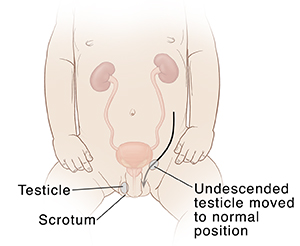
If your child's testicle doesn’t descend on its own, it should be treated to prevent future problems. Surgery is done to bring an undescended testicle into the normal position within the scrotum. An undescended testicle is the most common genital disorder identified at birth.
Why treatment is needed
-
The longer a testicle remains outside the scrotum, the more likely it is that it will produce fewer sperm.
-
An undescended testicle has a slightly higher risk of cancer in adulthood. This is true even after the testicle is brought down into the scrotum. But bringing the testicle down makes a problem easier to find.
-
An undescended testicle can leave a small tear (hernia) in the wall between the abdomen and the groin. The hernia needs to be treated to prevent future problems.
Surgery
The testicle is brought down into the scrotum during surgery.
-
You and your child are asked to arrive at the hospital or surgery center 1 to 2 hours before surgery.
-
Anesthesia is given to keep your son comfortable.
-
An opening (incision) is made in the groin or abdomen. Another small incision is made in the scrotum.
-
The testicle is detached from the tissue around it. Then it's brought down and stitched to the wall of the scrotum.
After surgery
Your child will most likely go home a few hours after surgery. They should be feeling better in 2 to 3 days.
-
Your child's healthcare provider may prescribe medicine to relieve any pain your child has. Be sure to use it as directed.
-
Your child should only have sponge baths for the first 1 to 2 days and then resume normal bathing activities, or as directed by your child's healthcare provider.
-
Most children will have one incision in the groin and a second incision in the scrotum. These are closed with skin glue. The glue will gradually flake off. You don't need to do any special care for the incisions. Stitches will dissolve as your child resumes their normal bathing activities. If removable stitches are used, they will need to be removed 7 to 10 days after surgery by your child's healthcare provider.
-
It's normal for the scrotum to appear swollen and bruised around the scrotal incision. This will all resolve with time and usually appear much better in a week.
-
Your child should not swim in a pool or lake water for 1 to 2 weeks after surgery, or as advised by your child's healthcare provider.
-
Light activity is fine, but your child should not participate in strenuous activities like sports for 3 to 4 weeks after surgery, or as directed by your child's healthcare provider.
When to call your child's healthcare provider
Call your child's healthcare provider right away if your otherwise healthy child has any of the signs or symptoms described below:
-
The incision bleeds or becomes red, or there is discharge from the incision
-
The child cries all the time, is unusually drowsy, or looks very ill
-
Other symptoms such as an unexplained rash, vomiting, or diarrhea
-
Fever (see Fever and children, below)
-
Seizure due to fever
Fever and children
Use a digital thermometer to check your child’s temperature. Don’t use a mercury thermometer. There are different kinds and uses of digital thermometers. They include:
-
Rectal. For children younger than 3 years, a rectal temperature is the most accurate.
-
Forehead (temporal). This works for children age 3 months and older. If a child under 3 months old has signs of illness, this can be used for a first pass. The provider may want to confirm with a rectal temperature.
-
Ear (tympanic). Ear temperatures are accurate after 6 months of age, but not before.
-
Armpit (axillary). This is the least reliable but may be used for a first pass to check a child of any age with signs of illness. The provider may want to confirm with a rectal temperature.
-
Mouth (oral). Don’t use a thermometer in your child’s mouth until they are at least 4 years old.
Use a rectal thermometer with care. Follow the product maker’s directions for correct use. Insert it gently. Label it and make sure it’s not used in the mouth. It may pass on germs from the stool. If you don’t feel OK using a rectal thermometer, ask the healthcare provider what type to use instead. When you talk with any healthcare provider about your child’s fever, tell them which type you used.
Below is when to call the healthcare provider if your child has a fever. Your child’s healthcare provider may give you different numbers. Follow their instructions.
When to call a healthcare provider about your child’s fever
For a baby under 3 months old:
-
First, ask your child’s healthcare provider how you should take the temperature.
-
Rectal or forehead: 100.4°F (38°C) or higher
-
Armpit: 99°F (37.2°C) or higher
-
A fever of ___________as advised by the provider
For a child age 3 months to 36 months (3 years):
-
Rectal or forehead: 102°F (38.9°C) or higher
-
Ear (only for use over age 6 months): 102°F (38.9°C) or higher
-
A fever of ___________ as advised by the provider
In these cases:
-
Armpit temperature of 103°F (39.4°C) or higher in a child of any age
-
Temperature of 104°F (40°C) or higher in a child of any age
-
A fever of ___________ as advised by the provider
Online Medical Reviewer:
Marc Greenstein MD
Online Medical Reviewer:
Raymond Kent Turley BSN MSN RN
Online Medical Reviewer:
Rita Sather RN
Date Last Reviewed:
12/1/2022
© 2000-2024 The StayWell Company, LLC. All rights reserved. This information is not intended as a substitute for professional medical care. Always follow your healthcare professional's instructions.